Reversing Severe Pulmonary Hypertension with Prolonged IABP Support: An Editorial Perspective
This opinion editorial explores a groundbreaking case where prolonged intra-aortic balloon pump (IABP) support successfully reversed severe pulmonary hypertension, ultimately enabling heart transplantation. We will take a closer look at this intricate case, discuss the key measures that contributed to its success, and provide insights into how modern cardiac care can overcome some of the more confusing bits and tricky parts of managing patients with end-stage heart failure complicated by severe pulmonary hypertension.
Although heart transplantation has long been the key treatment for those with end-stage heart failure, elevated pulmonary pressures pose intimidating challenges that have traditionally left both clinicians and patients facing uncertain outcomes. In this case, a 58-year-old man with severe heart failure and critically high pulmonary pressures benefited from prolonged IABP support, proving that even when confronted with tangled issues, dedicated preoperative optimization can yield remarkable improvements.
Heart Transplantation Amidst Intimidating Pulmonary Challenges
Severe pulmonary hypertension (PH) is known for its nerve-racking effects on heart transplantation outcomes. When pulmonary pressures are sky-high, post-transplant complications, especially right ventricular dysfunction, can be a nerve-racking prospect for clinicians. International guidelines define such severe PH as a relative contraindication for heart transplantation—a rule that underscores how on edge and full of problems this condition can be.
In the reported case, right heart catheterization revealed extremely high pressures. With a pulmonary artery systolic pressure (PASP) of 98 mmHg, a mean pulmonary artery pressure (mPAP) of 58 mmHg, and a pulmonary vascular resistance (PVR) approaching 9.78 Wood units, the patient’s condition appeared laden with issues that could easily have derailed a successful transplantation. The challenge was to manage these complicated pieces and bring down these values to a range that would not put the donor heart at risk.
Strategizing preoperative care: Extended IABP Support as a Game Changer
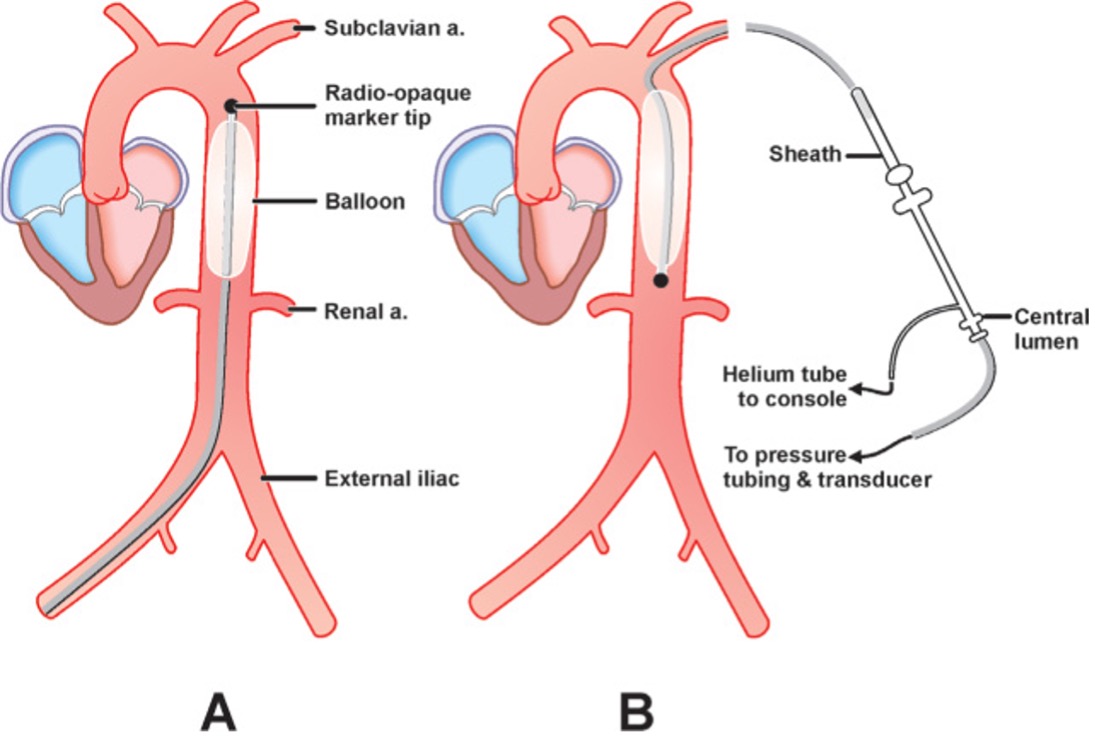
One of the key super important elements in this case was the use of prolonged IABP support over 62 days. This mechanical circulatory assistance device works by reducing cardiac afterload, thereby easing the workload on the heart and reducing pulmonary pressures. This approach not only helped in managing the tricky parts of severe PH through targeted therapy but also provided a bridge to heart transplantation that was previously seen as off-putting due to the high risks involved.
The case revealed that with a consistent approach combining IABP with optimal fluid management and targeted medications, the patient’s hemodynamic parameters improved dramatically. After 62 days, the PASP fell to 31 mmHg, mPAP to 24 mmHg, and the PVR to 4.85 Wood units—parameters that were well below the threshold for surgical contraindication. These improvements exemplify that even when facing complex issues, prolonged support with IABP can tilt the balance in favor of successful outcomes.
Key Elements of Preoperative Optimization in Cardiac Failure and PH
Managing a case like this requires handling many subtle parts and small distinctions with finesse. The preoperative phase featured several essential strategies:
- Fluid Management: Strict control of the fluid balance, achieved with diuretic therapy including furosemide and spironolactone, ensured that cardiac preload was maintained at optimal levels without exacerbating pulmonary congestion.
- Targeted Drug Therapy: Medications such as recombinant human brain natriuretic peptide and macitentan were administered to aid in cardiac recovery and lower pulmonary pressures. These medications helped tackle the nerve-racking elevated pulmonary pressures and supported the reversal of PH.
- Continuous Monitoring: Regular imaging studies and invasive hemodynamic monitoring—using both echocardiography and right heart catheterization—enabled the medical team to track progress meticulously, which is crucial when the situation is full of tricky parts.
This multi-pronged approach ensured that all the fine points were addressed. It is a model for how to take a closer look at all the subtle details and manage your way through the twists and turns of preoperative care in patients with severe cardiac conditions.
Comparing IABP to Other Mechanical Support Options
When considering mechanical circulatory support in patients with severe heart failure and pulmonary hypertension, alternatives such as left ventricular assist devices (LVAD) and extracorporeal membrane oxygenation (ECMO) are often brought into the discussion. Although these devices have their merits, the simplicity and effectiveness of IABP use in this case highlight its unique advantages.
Several reasons back the preference for IABP in this context:
- Simplicity: IABP is relatively easy to insert and adjust compared to more complicated devices like LVAD, which can be coupled with several tangled issues regarding device placement and management.
- Immediate Impact: IABP supports rapid reduction in cardiac afterload, a crucial factor when outcomes depend on quickly reversing high pulmonary pressures.
- Cost-Effectiveness and Accessibility: In many centers, IABP is a more readily available resource, making it a super important modality when immediate support is needed while waiting for additional resources.
By offering an effective bridge to transplantation, IABP has shown that even when other options appear intimidating, sometimes the more straightforward approach is the best to manage complicated pieces.
Dissecting the Surgical Procedure and Postoperative Management
The surgical phase of the heart transplantation involved numerous steps that required a coordinated effort to address each of the tiny complicated bits effectively. The donor heart was harvested under general anesthesia, and after meticulous preservation in HTK solution, it was implanted into the recipient under cardiopulmonary bypass. The surgical procedure, detailed and technical, highlights the many subtle parts that must all align perfectly for a successful outcome.
Immediately after the surgery, one of the most nerve-racking challenges was managing the patient’s hemodynamic instability. On the day following the transplant, the patient experienced an increase in pulmonary pressures, with PASP rising to 53 mmHg. This spike required high doses of dopamine and norepinephrine to maintain circulation, emphasizing that postoperative management can be as tricky as the preoperative phase.
To address these sudden shifts, the following strategies were deployed:
- High-Dose Inhaled Nitric Oxide: Administered at 17 ppm, inhaled nitric oxide played a key role in reducing the right ventricular afterload by dilating the pulmonary vasculature.
- Additional Vasopressor Support: Adjustments in vasopressor dosage helped in stabilizing the patient’s hemodynamics during the critical early postoperative period.
- Targeted Drug Therapy: Continual use of agents such as milrinone and macitentan ensured that pulmonary pressures remained within an acceptable range.
- Meticulous Fluid Management: As in the preoperative phase, controlling fluid balance helped prevent volume overload and further pulmonary congestion.
These measures, combined with persistent monitoring through echocardiography, ultimately led to a smooth recovery. By the ninth postoperative day, the patient was transferred out of the ICU, and subsequent evaluations showed a substantial improvement in cardiac function, with left ventricular ejection fraction (LVEF) rising to near normal levels over time.
Understanding the Fine Points of Postoperative Hemodynamics
The period following heart transplantation is full of tricky parts and subtle details that need constant attention. Postoperatively, despite a temporary surge in pulmonary pressures, the medical team worked diligently to steer through the challenges. A comprehensive approach involving mechanical ventilation, close circulatory monitoring, and incremental adjustments in medication dosage helped in effectively managing these fine points.
Key hemodynamic parameters that indicated success included:
| Parameter | Before IABP Support | After 62 Days of IABP Support |
|---|---|---|
| PASP (mmHg) | 98 | 31 |
| mPAP (mmHg) | 58 | 24 |
| PVR (Wood Units) | 9.78 | 4.85 |
These numbers are not merely figures; they embody the palpable improvement in the patient’s condition and highlight how thorough pre- and postoperative management can successfully overcome even the most intimidating challenges.
Lessons Learned: Managing Your Way Through Complicated Cardiac Cases
This case offers a wealth of lessons for clinicians, patients, and policymakers alike. While the numerous twists and turns in managing severe pulmonary hypertension are on edge and often intimidating, this case reinforces that with rigorous, patient-centered strategies, a positive outcome is achievable. Some of the key takeaways include:
- Early Intervention is Critical: Addressing the elevated pulmonary pressures head-on with an immediate institution of IABP support can reverse the detrimental hemodynamic changes before they become irreversible.
- Precision in Fluid and Drug Management: A carefully customized regimen of diuretics and pulmonary pressure–lowering agents is essential. The success rests on finding your path through the subtle, confusing bits to achieve a balanced fluid status and optimal cardiac pressures.
- Continuous Monitoring: Frequent imaging studies and invasive monitoring form the backbone of a responsive treatment strategy. The ability to get into the nitty-gritty details of the patient’s progress cannot be overstated.
- Team-Based Approach: This case underscores the importance of coordinated care. From the cardiac surgeons and anesthesiologists to the critical care team and nursing staff, each contributor played a super important role in navigating through the tangled issues.
The interplay between these factors—mechanical support, meticulous fluid management, and tailored medication protocols—illustrates the power of modern medical technology when integrated with clinical expertise. It serves as an encouraging model for how even cases that seem overwhelming can be turned around with persistence and collaboration.
Exploring the Role of Lifestyle and Nutrition in Long-Term Recovery
While the transient postoperative phase demands intensive care, long-term recovery after heart transplantation also involves addressing lifestyle and nutritional factors. Patients recovering from severe heart failure and pulmonary hypertension must consider several key areas:
- Balanced Nutrition: A heart-healthy diet, low in salt and saturated fats, is essential. Patients should aim to include a variety of fruits, vegetables, whole grains, and lean proteins, which support both cardiovascular health and general well-being.
- Regular Physical Activity: Tailored rehabilitation programs are an essential part of recovery, helping patients rebuild strength and improve circulatory efficiency. Exercise regimens should consider the individual’s capacity and gradually increase in intensity.
- Stress Management: Techniques for stress reduction, including yoga, meditation, or gentle physical activities like walking, can prove beneficial. These methods assist in managing the nerve-racking psychological aspects that often accompany severe medical conditions.
- Regular Follow-Up: Regular check-ups, including echocardiograms and consultation with cardiac specialists, ensure that any subtle changes can be caught early and managed appropriately.
The focus on lifestyle and nutritional adjustments is a reminder that successful heart transplantation is not solely the result of surgical precision and mechanical devices. Instead, it is a holistic process that requires patients to take an active role in their recovery, navigating the long journey post-surgery with sustained care and support.
The Future of Cardiac Support: Research and Clinical Trials
One of the most exciting aspects of this case is its potential to influence future research and clinical practice. While the successful reversal of pulmonary hypertension with prolonged IABP support in this patient is promising, it also raises several key questions that future studies must address:
- The Optimal Timing and Duration: What is the ideal moment to initiate IABP support, and how long should it be maintained to yield the best results without risking further complications?
- Comparative Effectiveness: How does IABP compare with other forms of mechanical circulatory support, such as LVADs or ECMO, especially in the context of patients with severe pulmonary hypertension?
- Patient Selection Criteria: Which subset of patients might benefit the most from this approach? Future large-scale, multi-center randomized controlled trials can help refine these criteria further.
- Cost-Effectiveness and Accessibility: Beyond clinical outcomes, there is a need to assess the financial implications and resource availability, which are critical when considering the broader implementation of this strategy.
By addressing these subtle details and tricky parts, future research can potentially broaden the applicability of this promising intervention, offering hope to many who face nerve-racking pulmonary challenges before heart transplantation.
Personalizing Cardiac Care: A Patient-Centered Approach
A key takeaway from this case is the significance of individualized care. Every patient presents with a unique set of circumstances—riddled with tension and unpredictable turns—that can influence both treatment strategies and outcomes. Personalized medicine in the context of heart failure and pulmonary hypertension can involve:
- Tailoring Interventions: Adjusting mechanical support durations, fluid management protocols, and drug regimens to meet the individual needs of each patient.
- Comprehensive Risk Assessment: Using scoring models, such as the Seattle Heart Failure Model mentioned in this case, to evaluate both short-term and long-term risks, thereby guiding clinical decision-making.
- Engaging Patients: Involving the patient and their family in the treatment process, ensuring that they understand the twists and turns of the treatment plan so that they can be active participants in their recovery journey.
- Long-Term Monitoring: Implementing scheduled follow-ups and regular imaging studies to catch any slight differences in cardiac function before they escalate into major complications.
This patient-centered paradigm not only improves clinical outcomes but also empowers patients by providing them with the tools and knowledge necessary to manage their own recovery. Ultimately, it is this partnership between clinician and patient that lays the foundation for a successful, lasting recovery following such an intricate procedure.
Looking Ahead: Integrating Alternative Medicine and Nutrition in Cardiac Recovery
While conventional treatments continue to be the cornerstone of managing complex cardiac cases, there is growing interest in complementary approaches that incorporate modern alternative medicine and nutrition. Some of the ways these disciplines can support recovery include:
- Herbal Supplements and Anti-Inflammatory Agents: Certain herbal extracts and supplements have anti-inflammatory properties that may help reduce oxidative stress and improve cardiovascular health. However, it is essential to discuss any such additions with healthcare providers to avoid interference with critical medications.
- Nutritional Therapy: A nutritional plan rich in antioxidants, omega-3 fatty acids, and essential minerals can bolster cardiac function. Medical nutrition therapy is becoming an increasingly recognized adjunct to conventional heart failure treatments.
- Mind-Body Interventions: Practices such as meditation, acupuncture, and gentle yoga can assist those dealing with the challenging parts of recovery. These interventions help calm the mind while positively affecting the physiological state, supporting overall well-being during the recovery journey.
Integrating these alternative approaches into the standard of care may aid in addressing the small distinctions and subtle parts in patient recovery that are not solely resolved by surgical or pharmacological interventions.
Conclusion: Finding Your Way Through the Tangled Issues of Cardiac Transplantation
This case stands as a testament to the power and potential of prolonged IABP support in reversing severe pulmonary hypertension, even in the face of nerve-racking challenges associated with heart transplantation. By combining prolonged mechanical support, meticulous fluid management, and tailored drug therapy, the medical team was able to transform a situation once thought to be on edge into an opportunity for successful transplantation.
It is clear that managing these confusing bits requires a holistic and multi-faceted approach—not only addressing the immediate cardiac needs but also preparing for long-term recovery through lifestyle modifications, patient education, and innovative research. The use of IABP in this context provides clinicians with a tool to steer through the minor twists and turns of hemodynamic management and improve outcomes in patients who might otherwise be ruled out as transplant candidates.
As we look ahead, this experience encourages further exploration into optimizing mechanical circulatory support, personalizing cardiac care, and integrating complementary therapies. By addressing every fine point—be it through meticulous preoperative management or comprehensive postoperative care—we can chart a clearer, more hopeful pathway for patients facing the daunting challenges of severe pulmonary hypertension and heart failure.
Ultimately, this case is not just a story of medical success; it is a narrative of perseverance, collaboration, and innovation. It demonstrates that even when the road is full of tricky parts and nerve-racking obstacles, the commitment to finding your way through can rewrite the expected outcomes of heart transplantation.
By continuously focusing on the essential issues, engaging in ongoing research, and delivering patient-centered care, the healthcare community can transform even the most intimidating cases into opportunities for life-saving breakthroughs. As we continue to build on this experience, the lessons learned here will undoubtedly help shape a future where no patient is ever doomed by complicated pieces or on edge challenges—instead, every patient receives the chance to embark on a new journey toward renewed health.
Originally Post From https://cardiothoracicsurgery.biomedcentral.com/articles/10.1186/s13019-025-03598-1
Read more about this topic at
Intra-Aortic Balloon Pump Bridging to Heart Transplantation
P.502: Use of the intra-aortic balloon pump as a bridge to …